An international team of researchers led by scientists from the University of Illinois has developed an ultra-thin, wearable epidermal sensing device that measures vascular and tissue health by mapping blood flow. The device provides insight that will enable healthcare providers to better monitor conditions like wound healing and skin grafts and improve treatment of diseases such as diabetes and arthritis. Providing reliable, continuous, and noninvasive monitoring of both larger vessels and the tiny vessels found close to the surface of the skin, the soft, skin-conforming electronics deliver a level of accuracy unattainable by competing technologies.
“Our device is much like a kid’s temporary tattoo, in terms of its form factor,” says John Rogers, one of the developers of the device and a professor of engineering and materials science at the University of Illinois at Urbana-Champaign. “It laminates directly onto the skin, and operates in a non-optical mode, via thermal analysis.”
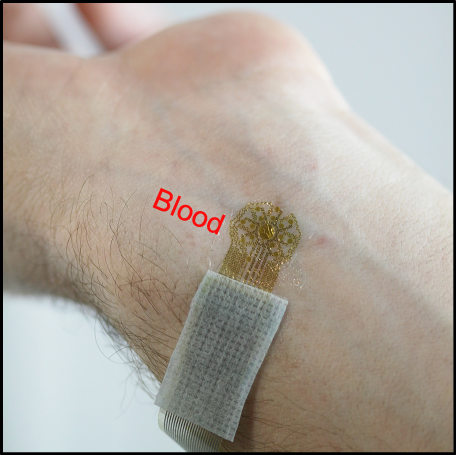 Researchers have developed an ultra-thin, wearable epidermal sensing device that resembles a temporary tattoo that measures vascular and tissue health by mapping blood flow. The device provides physicians with information that advances wound care and treatment of a wide range of diseases. (Source: R. Chad Webb, Department of Materials Science and Engineering, University of Illinois at Urbana-Champaign)
Researchers have developed an ultra-thin, wearable epidermal sensing device that resembles a temporary tattoo that measures vascular and tissue health by mapping blood flow. The device provides physicians with information that advances wound care and treatment of a wide range of diseases. (Source: R. Chad Webb, Department of Materials Science and Engineering, University of Illinois at Urbana-Champaign)
The skin interface eliminates false readings that can be generated as a result of movement of the targeted area.
It’s in the Blood
These measurements allow healthcare professionals see early-warning signs that other techniques often miss. For example, an overabundance of blood flow to the near-surface regions of the skin can indicate inflammation from infection or an allergic reaction. On the other hand, a decrease in the perfusion of blood points to diseases like hardening of the arteries, heart failure, and diabetes.
The longer the duration of visibility, the more complete the picture. Tracking blood flow over an entire day enables doctors to see variations in perfusion that a briefer snapshot would miss. The better doctors can monitor these conditions, the better they can tailor their treatment regimens. This is exactly what the new epidermal sensing device aims to do.
Looking a Little Deeper
The blood flow monitor combines ultra-thin layers of gold, chromium, and copper to create a central circular thermal actuator measuring 1.5 mm, surrounded by a radial array of temperature sensors. The flexible electronics reside on a 40-micrometer-thick layer of silicone, which acts as a substrate.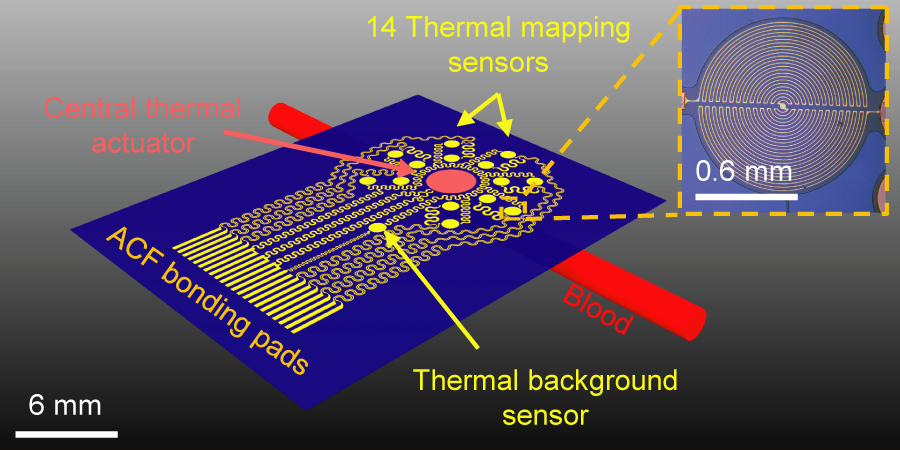 The epidermal sensing device combines a thermal actuator and a radial array of 14 temperature sensors made of ultra-thin layers of gold, chromium, and copper, providing the flexibility required to allow the device to comfortably conform to the surface of the skin. (Source: R. Chad Webb, Department of Materials Science and Engineering, University of Illinois at Urbana-Champaign)
The epidermal sensing device combines a thermal actuator and a radial array of 14 temperature sensors made of ultra-thin layers of gold, chromium, and copper, providing the flexibility required to allow the device to comfortably conform to the surface of the skin. (Source: R. Chad Webb, Department of Materials Science and Engineering, University of Illinois at Urbana-Champaign)
To ensure accurate measurements, the sensor rests on top of the skin without distorting the blood flow, held tightly against the skin by an electrostatic interaction called van der Waals forces. The attraction precludes any movement between the sensor and skin, which reduces the chances of false readings. Users can add medical tape to provide an extra measure of stability.
To measure blood flow in the outermost 1 to 2 mm of skin, the blood flow monitor’s thermal actuator generates heat up to 6-7 degrees Celsius, imperceptibly warming the skin. Blood in vessels beneath the device carry away the heat. The sensors around the actuator measure the direction of blood flow and the dissipation of the heat, with accuracy to within 0.01 degrees Celsius.
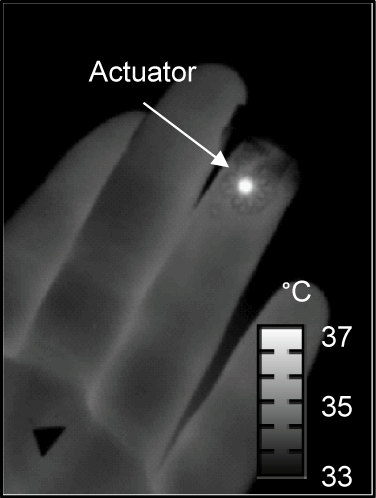 The thermal actuator in the epidermal sensing device generates heat up to 7 degrees Celsius, imperceptibly warming the skin. Blood in vessels beneath the device carry away the heat, and the device’s sensors measure the direction of blood flow and the dissipation of the heat. (Source: R. Chad Webb, Department of Materials Science and Engineering, University of Illinois at Urbana-Champaign)
The thermal actuator in the epidermal sensing device generates heat up to 7 degrees Celsius, imperceptibly warming the skin. Blood in vessels beneath the device carry away the heat, and the device’s sensors measure the direction of blood flow and the dissipation of the heat. (Source: R. Chad Webb, Department of Materials Science and Engineering, University of Illinois at Urbana-Champaign)
Computer algorithms compare the sensor data with fluid dynamic models of blood flow and quantitatively determine the heat pattern differences as the heat dissipates.
Flawed Alternatives
One of the drivers for the development of the epidermal sensor lies in the shortcomings of existing acoustic- and optical-based blood flow monitoring technologies. These methods have proven to be extremely sensitive to motion, requiring testing to take place at a clinic or hospital, where the patient must remain still during the imaging procedure. The optical technique’s sensitivity stems from the way that the directionality and magnitude of scattered light affects accuracy.
Wearable optical measurement systems have become available, but their rigid, bulky components have proven to be too uncomfortable to be effective for prolonged testing, and the pressure they put on the body can cause erroneous readings.
In contrast, the thermal-based blood flow monitor provides accurate readings even if movement comes into play. The device attaches to the skin like a temporary tattoo, enabling accurate 24-hour monitoring of blood flow wherever a patient is. In addition, the design is simpler and less expensive to produce.
More Work to Do
While the epidermal sensing system promises to greatly improve healthcare in a number of key areas, the researchers have more testing and development to do before it can be commercialized.
Currently, the system can only provide visibility to a depth of 2 mm. The group hopes to extend that range by configuring the sensors and thermal actuator in new ways.
The team also wants to integrate a self-contained power source and wireless communications into the unit. “We are working to integrate these sensors into a fully wireless system, for continuous recording and monitoring,” says Roger

